Progesterone is far more than a reproductive hormone. It's a foundational pillar for your long-term health, acting as a master regulator for your mood, sleep quality, and overall vitality. While its levels naturally ebb and flow throughout your life, understanding its role is less about a single "average progesterone level" and more about optimizing its function for healthy ageing.
Why Progesterone Levels Are a Cornerstone of Your Longevity

It’s easy to pigeonhole progesterone as just a "pregnancy hormone," but its influence reaches far beyond fertility, acting as a true cornerstone of healthy ageing. Think of it as a vital biological regulator. When levels are balanced, it helps create a sense of calm, promotes deep, restorative sleep, and supports sharp cognitive function—all critical components for a long and vibrant life.
This guide is designed to reframe how you see progesterone. It's not just a number on a lab report, but a key player in your personal longevity strategy. We'll explore how keeping your levels in their optimal range contributes directly to your vitality, giving you actionable knowledge to feel your best for decades to come. Mastering this hormone is a proactive step toward taking control of your long-term wellbeing.
The Symphony of Your Health
To truly appreciate its importance, picture progesterone as a calming influence in an orchestra. When it's present in the right amount, every instrument plays in harmony, creating a beautiful, balanced sound. In the same way, balanced progesterone helps coordinate countless bodily functions, directly impacting your longevity by:
- Improving Sleep Quality: It has a natural calming effect, helping you achieve the deep, restorative rest essential for cellular repair and brain health.
- Enhancing Mood Stability: By gently modulating brain chemistry, it can help mitigate the chronic stress and anxiety that accelerate ageing.
- Strengthening Cognitive Function: It plays a protective role in the brain, supporting memory and focus, which are key to maintaining mental sharpness as you age.
Understanding Progesterone Numbers
For a quick reference, here are the typical progesterone ranges you can expect to see at different stages of life.
Progesterone Levels At-a-Glance
| Life Stage / Cycle Phase | Typical UK Progesterone Range (nmol/L) |
|---|---|
| Men (Post-Puberty) | < 1.0 nmol/L |
| Women (Follicular Phase) | < 2 nmol/L |
| Women (Luteal Phase Peak) | 16 – 60 nmol/L |
| Women (Post-Menopause) | < 1.0 nmol/L |
These figures give us a snapshot, but the story behind them is what truly matters for your long-term health.
Historically, the main focus of quantifying average progesterone levels has been within reproductive medicine. UK-based research and large-scale health surveys have been instrumental in establishing the reference ranges we use today. These studies were crucial in identifying the typical mid-luteal phase peak values, which generally fall between 5 to 20 ng/mL (that’s about 15.9 to 63.6 nmol/L). This was a significant step forward in understanding female hormonal health.
Progesterone isn’t just a hormone; it's a fundamental biomarker of your body's internal balance. Monitoring it provides a window into your current health and offers vital clues for optimising your future longevity.
As a crucial hormone, progesterone is just one of many important indicators of your body's overall status. To get a fuller picture, you might be interested in our guide on what blood biomarkers show about your health. This guide will empower you to understand not just progesterone, but the entire ecosystem of hormones that defines your unique health journey.
The Hidden Roles of Progesterone in Healthy Ageing
Most people know progesterone as a pregnancy hormone, but its job description is far wider, playing a crucial part in healthy ageing long after the reproductive years are over. Think of it as a quiet, multitasking force working to preserve your vitality.
Understanding what this hormone does behind the scenes explains why maintaining balanced average progesterone levels is so vital for your long-term health. It influences everything from the strength of your skeleton to your ability to get a good night's sleep—two pillars of longevity.
Supporting Stronger Bones
One of progesterone’s most underrated roles is in maintaining bone health. We often hear about oestrogen’s job in preventing bone breakdown, but progesterone is the builder. It actively stimulates osteoblasts—the cells responsible for creating new bone tissue.
This teamwork between oestrogen and progesterone is essential for keeping your skeleton dense and resilient. As progesterone levels dip, particularly during perimenopause and beyond, the signal to build new bone weakens. This can tip the scales towards bone loss, raising the long-term risk of osteopenia and osteoporosis. Maintaining adequate progesterone is a proactive strategy for skeletal strength.
Achieving Deeper, More Restorative Sleep
Ever wondered why quality sleep becomes more elusive as you get older? Progesterone is a key part of the puzzle. It has a wonderfully calming effect on the brain, acting almost like a natural sedative.
How does it work? Progesterone interacts with the brain's GABA receptors, the very same ones targeted by many sleep aids.
GABA (gamma-aminobutyric acid) is your body’s main "chill-out" neurotransmitter. It quiets down mental noise, making it easier to relax and fall asleep. Deep sleep is when your body performs critical repair and detoxification processes essential for longevity.
When your progesterone is at a healthy level, this effect helps you get that restorative sleep. As levels decline with age, this calming influence wanes, which is a major reason why many people struggle with sleep during menopause, impacting their long-term health.
Protecting Your Brain and Mood
Beyond sleep, progesterone is a key player in brain health and a crucial element for cognitive longevity. It acts as a neuroprotective agent, shielding nerve cells from damage and reducing inflammation. It also supports the myelin sheath, the protective coating around your nerves that ensures your brain’s wiring works efficiently.
This has huge implications for preserving cognitive function as you age. On top of that, by working with GABA, progesterone helps soothe the nervous system and manage stress. Stable levels can lead to a better mood and less anxiety, reducing the chronic stress that can accelerate the ageing process.
But that’s not all. Progesterone also contributes to longevity through:
- Skin Health: It helps keep skin elastic and hydrated by supporting collagen production.
- Thyroid Function: It helps your body properly utilise thyroid hormones, which are the masters of your metabolism and energy.
- Cardiovascular Support: It encourages blood vessels to relax, which helps in maintaining healthy blood pressure.
When you see all these hidden jobs, it’s clear that progesterone is a foundational element for feeling strong, sharp, and well for decades.
Progesterone’s Monthly Rhythm: A Guide to Your Menstrual Cycle
Getting to know your menstrual cycle is like learning the unique language your body speaks. Progesterone is a major character in this conversation, with its levels rising and falling in a predictable pattern that affects everything from your fertility to how you feel day-to-day.
Think of your cycle as a story unfolding in two distinct halves. In the first part, progesterone stays quietly in the background, letting other hormones run the show. But in the second half, it steps firmly into the spotlight, completely changing your body's internal environment to prepare for a potential pregnancy.
The Follicular Phase: Laying the Groundwork
The first day of your period kicks off the follicular phase. Right now, your body’s main job is to get an egg ready for release. To do this, progesterone levels stay very low—and that's exactly what's needed.
This quiet period for progesterone allows oestrogen to take the lead, building up a lush uterine lining. Low progesterone at this stage is not just normal; it’s essential for the whole process to work.
The Luteal Phase: The Big Surge
Everything shifts after ovulation. The tiny sac (follicle) that released the egg transforms into a temporary gland called the corpus luteum, which is basically a progesterone-making machine. This is the start of the luteal phase.
Progesterone levels now shoot up. This surge is vital for making the uterine lining thick, stable, and welcoming for a fertilised egg. It’s also this hormonal shift that often brings on premenstrual symptoms like mood changes or tender breasts.
This dramatic rise and fall is the defining feature of progesterone’s role in the cycle.
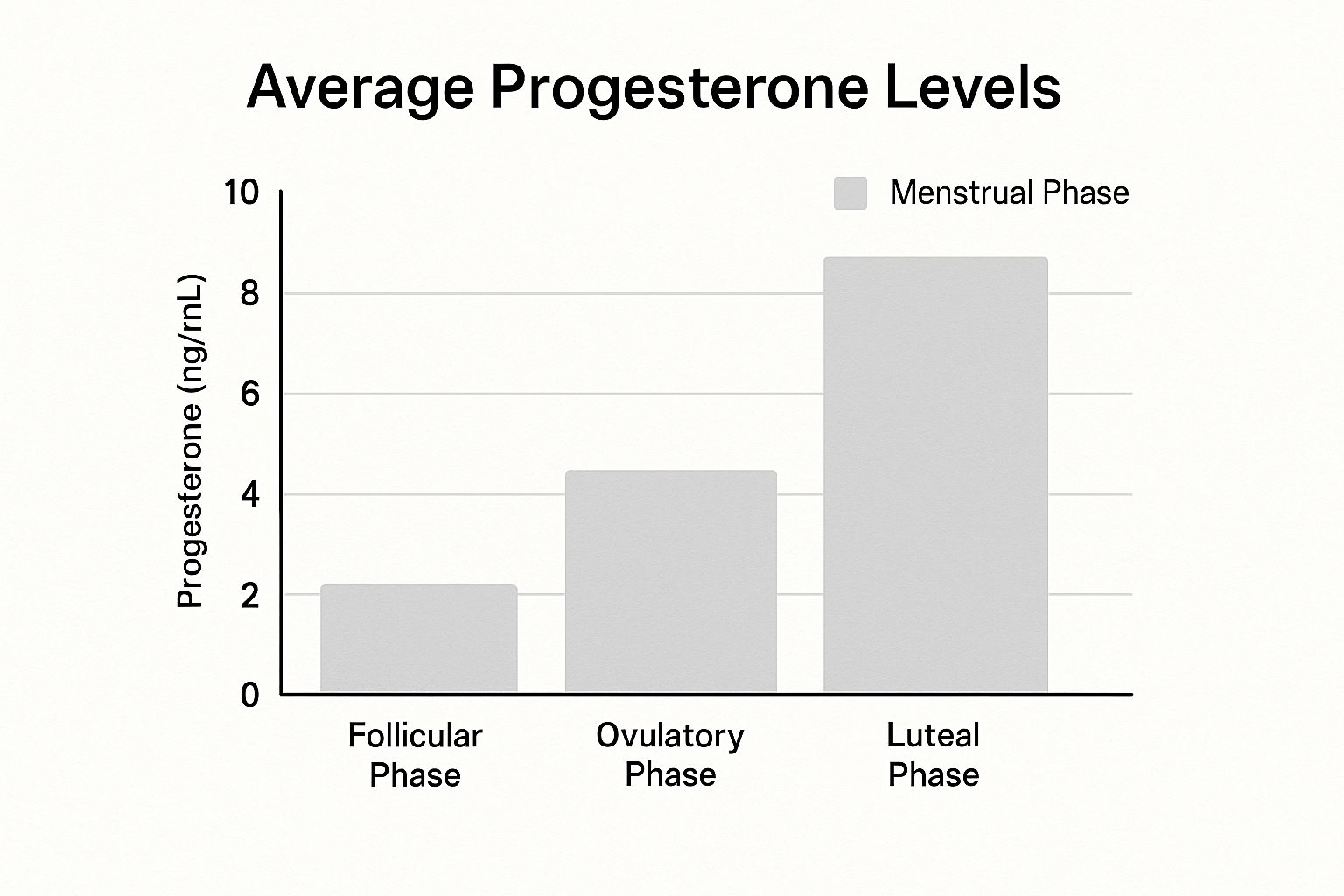
As you can see, progesterone jumps from a barely-there level in the follicular phase to its peak during the second half of the cycle.
This table gives a clearer picture of what the numbers look like in the UK.
Average UK Progesterone Levels by Menstrual Cycle Phase
| Menstrual Phase | Day Range (Approx.) | Typical UK Range (nmol/L) | What This Level Indicates |
|---|---|---|---|
| Follicular Phase | Day 1–14 | < 4 nmol/L | Oestrogen is dominant, preparing the follicle and uterine lining. Progesterone is correctly low. |
| Ovulation | Day 14–16 | 4 – 10 nmol/L | The initial rise signals that the egg has been released and the corpus luteum is forming. |
| Luteal Phase | Day 15–28 | > 12 nmol/L | The corpus luteum is active, producing high progesterone to sustain the uterine lining for potential pregnancy. |
| Luteal Phase Peak | Day 21 (approx.) | > 30 nmol/L | A level above 30 nmol/L around 7 days post-ovulation is considered strong proof that ovulation occurred. |
Understanding these ranges is key to interpreting your own test results and knowing what's happening inside your body.
Why Timing Your Progesterone Test Is Everything
Because its levels fluctuate so much, when you test for progesterone is absolutely crucial. A test done early in your cycle will naturally show a low number, but that’s not a sign of a problem—it’s just what’s supposed to happen.
The best time to test is mid-way through the luteal phase. This is usually around day 21 of a 28-day cycle, or more accurately, about seven days after you think you ovulated.
A high level at this point is the confirmation you’re looking for: your body successfully released an egg. If the result is low during this peak window, it could suggest ovulation didn't happen, giving you a vital piece of information to discuss with your doctor.
For those wanting to support their reproductive health, other approaches can offer valuable insights. For example, the principles of Traditional Chinese Medicine for fertility can provide a different perspective on creating hormonal balance. Seeing your cycle as a predictable pattern, not a mystery, is the first step towards taking charge of your health.
Progesterone Shifts During Pregnancy and Perimenopause

Beyond the monthly menstrual cycle, two major life events trigger the most dramatic shifts in progesterone: pregnancy and perimenopause. These are profound hormonal transitions, each with a unique purpose. Understanding these changes is key to managing your health not just in the moment, but for your long-term vitality.
Think of pregnancy as a hormonal marathon where progesterone builds to an incredible peak to support new life. In contrast, perimenopause is a gradual winding down, where the once-reliable surge of progesterone becomes less predictable before it declines. Both stages are natural, but knowing what to expect empowers you to navigate them with confidence and foresight for your future health.
Progesterone: The Protector of Pregnancy
During pregnancy, progesterone’s job description changes completely. It goes from being a cycle regulator to the primary guardian of the pregnancy itself. Its levels skyrocket, produced first by the corpus luteum and then taken over by the placenta. This sustained, high level of progesterone is absolutely essential for maintaining a healthy pregnancy.
This surge performs several vital roles. It relaxes the uterus's smooth muscles to prevent premature contractions, supports the growth of uterine blood vessels to nourish the foetus, and even helps prepare the breasts for milk production. UK data clearly shows this steady, substantial increase. For instance, in the first trimester, average progesterone concentrations range from 10 to 44 ng/mL (31.8 to 139.9 nmol/L).
This then climbs significantly in the second trimester to about 19.5 to 82.5 ng/mL (62 to 262 nmol/L). By the third trimester, levels can peak anywhere between 65 and 290 ng/mL (207 to 923 nmol/L). You can explore more about these pregnancy progesterone levels on blog.inito.com.
Monitoring these levels is a key part of prenatal care, helping to confirm the viability of the pregnancy. For anyone planning a family, understanding these hormonal requirements is vital, and specialised tools like a pregnancy blood test can offer clear insights.
"During pregnancy, progesterone becomes the master architect of the uterine environment. Its steady rise is not just a number on a lab report; it’s a direct indicator of the body’s commitment to sustaining a new life."
This period truly highlights progesterone’s powerful influence, showcasing its role as a fundamental hormone for both creating and sustaining life. Without this dramatic increase, a successful pregnancy simply wouldn't be possible.
The Perimenopausal Decline: A New Hormonal Landscape
Perimenopause, the transition to menopause, marks the beginning of a major hormonal shift. This phase, which can last for several years, is defined by fluctuating and ultimately declining progesterone levels. The ovaries become less consistent in releasing eggs, leading to more anovulatory cycles where ovulation doesn't happen at all.
Because progesterone is mainly produced after ovulation, these cycles mean less progesterone gets made. This creates a state of hormonal imbalance, often called "oestrogen dominance," where oestrogen levels are relatively higher than progesterone. This imbalance is directly responsible for many classic perimenopausal symptoms that can impact long-term health if left unmanaged.
Here are common experiences linked to falling progesterone, and their longevity implications:
- Irregular Cycles: As progesterone becomes erratic, periods can become longer, shorter, heavier, or lighter.
- Sleep Disturbances: The calming, sleep-promoting effects of progesterone diminish, contributing to insomnia. Chronic poor sleep is a major accelerator of ageing.
- Increased Anxiety and Mood Swings: With less progesterone to support the brain’s calming GABA pathways, feelings of anxiety and irritability can intensify, increasing chronic stress.
- Hot Flushes and Night Sweats: The imbalance caused by low progesterone can contribute to these vasomotor symptoms, disrupting sleep and quality of life.
Navigating this transition is a key part of healthy ageing. Understanding that symptoms like anxiety or poor sleep are rooted in these hormonal shifts is the first step toward finding effective management strategies and supporting your long-term wellbeing.
How to Test and Understand Your Progesterone Levels
Getting real answers about your progesterone levels is a straightforward process that empowers you to understand what’s happening inside your body. By getting tested, you swap guesswork for actionable data—a critical step in managing your long-term health and vitality.
The most common and reliable method is a simple blood test. This measures the exact amount of progesterone circulating in your bloodstream at a specific moment, giving you a precise snapshot. The procedure itself is simple, but when it comes to progesterone, timing is everything.
The Gold Standard: The Day 21 Blood Test
For anyone with a regular menstrual cycle, the “Day 21” blood test is the gold standard for a reason. It's strategically timed to catch your progesterone at its peak, which usually happens about seven days after you’ve ovulated.
If you have a textbook 28-day cycle, this falls on day 21. However, if your cycle is longer, say 35 days, your progesterone peak would be closer to day 28. The key is to test approximately seven days before you expect your next period. This timing is crucial because a high progesterone level confirms that ovulation has successfully occurred.
A progesterone level above 5 ng/mL (or roughly 16 nmol/L) on this day is generally considered solid proof of ovulation. For optimal fertility and to properly support a potential early pregnancy, however, many specialists really want to see levels of 10 ng/mL (32 nmol/L) or even higher.
This one test can tell you so much, confirming a fundamental part of your hormonal health.
Decoding Your Lab Report: Units and What They Mean
When your results come back, you’ll see numbers followed by units like nmol/L or ng/mL. They're just different ways of measuring concentration.
- nmol/L (nanomoles per litre): This is the standard unit you’ll see on lab reports from the NHS and labs across the UK and Europe.
- ng/mL (nanograms per millilitre): This unit is more common in the United States.
To convert ng/mL to the UK standard nmol/L, simply multiply by 3.18. For example, a result of 10 ng/mL is the same as about 31.8 nmol/L. Knowing this helps you compare your results to different reference ranges.
Other Ways to Test Progesterone
While a blood test gives you the most direct measurement, other methods can offer different insights, especially for tracking trends over time.
A popular alternative is a urine test, which measures PdG (pregnanediol glucuronide). In simple terms, PdG is what progesterone breaks down into before it leaves your body.
Here’s a quick rundown of how they stack up:
| Testing Method | The Good Bits | The Not-So-Good Bits |
|---|---|---|
| Serum Blood Test | Gives a highly accurate, single-moment snapshot. It's the clinical standard for confirming ovulation. | Only measures one point in time; requires a clinic visit or phlebotomy service. |
| Urine (PdG) Test | Super convenient for at-home use. It helps confirm the ovulation event by tracking levels over a few days. | Less precise than a blood test. It's measuring a by-product, not progesterone itself. |
With their convenience, at-home testing kits are becoming a go-to for many. If you're keen on getting a broader picture of your hormonal health from home, learning more about hormone level testing at home can open up practical options. These kits are a fantastic way to gather data and start a more informed conversation with your doctor about your longevity goals.
Ultimately, understanding your average progesterone levels isn’t just about fertility. It’s about taking proactive control of your long-term health for a more vibrant future.
Answering Your Progesterone Questions
Let's dive into some of the most common questions about progesterone. My goal is to give you clear, straightforward answers you can use on your health journey.
What Are the Signs of Low Progesterone?
Recognising the signs of low progesterone is your body's way of signalling an imbalance. The most obvious signs are irregular menstrual cycles, trouble conceiving, or spotting between periods.
However, its impact on your long-term health can show up in other ways. Low progesterone can manifest as persistent anxiety, poor sleep, or recurring headaches and migraines, especially before your period. Behind the scenes, progesterone helps calm the brain by supporting a neurotransmitter called GABA. When levels are low, it can leave you feeling anxious and unable to switch off at night. This isn't just a minor annoyance; chronic stress and poor sleep are well-known to accelerate the ageing process. While these symptoms are important clues, you'll always need to see a healthcare professional for a proper diagnosis.
Do Men Also Need to Worry About Progesterone?
Absolutely. It’s often seen as a "female" hormone, but progesterone plays a critical, often overlooked, role in men's health and longevity. Men produce it in smaller quantities, mainly in their adrenal glands and testes.
One of its key jobs in men is balancing testosterone and oestrogen. Progesterone is a precursor to testosterone and it also helps to counteract the effects of excess oestrogen. When a man's progesterone is too low, it can contribute to oestrogen dominance, leading to symptoms like fatigue, a low sex drive, and weight gain.
For men, balanced progesterone is part of the foundation for maintaining muscle mass, energy levels, and overall vitality as they age. It's a key player in the complex hormonal orchestra that supports long-term male health.
Recognising that progesterone is crucial for everyone gives us a much fuller picture of what hormonal health means for healthy ageing.
How Can I Support Healthy Progesterone Levels Naturally?
Encouraging your body’s own hormone production is a powerful strategy for long-term wellness. Several lifestyle shifts can create an environment where your hormones can thrive. The most impactful action you can take is stress management.
Your body uses the same building blocks to make both the stress hormone cortisol and progesterone. If you're constantly stressed, your body will prioritise making cortisol, essentially "stealing" the resources that should have gone to progesterone production. This is known as the "pregnenolone steal."
Here are actionable ways to support hormonal harmony for longevity:
- Prioritise Nutrient-Dense Foods: Focus on nutrients that support progesterone production, like Vitamin B6 (chicken, fish, potatoes), zinc (seeds, nuts), and magnesium (leafy greens, dark chocolate). A whole-foods diet is foundational.
- Actively Manage Stress: Incorporate practices like mindfulness, meditation, or gentle walks in nature. These activities help lower cortisol, freeing up the raw materials for progesterone.
- Maintain a Healthy Weight: Being significantly over or underweight can disrupt hormonal balance. Gentle, consistent exercise and a balanced diet are key.
These are supportive measures, not replacements for medical care. For those exploring general hormonal health, you might find useful insights by researching the top hormone balance supplements.
Is Progesterone Linked to Weight Gain?
This is a common worry, but progesterone itself doesn't directly cause you to gain fat. In fact, it has a mild diuretic effect, helping your body shed excess water.
The issue arises from hormonal imbalance—specifically, when progesterone is low compared to oestrogen. This state, known as oestrogen dominance, can lead to water retention and bloating, which makes you feel heavier. It's important to separate actual fat gain from this temporary, hormone-related fluid retention. Understanding how hormonal balance, diet, and lifestyle all work together is crucial for managing your body composition over the long run.
At Lola, we believe that understanding your body's unique chemistry is the key to unlocking your health potential. Our at-home and in-clinic blood tests provide a clear, comprehensive analysis of your biomarkers, reviewed by doctors to give you actionable insights for your longevity journey. Take control of your health today. Explore your testing options.


