When your blood test results show high neutrophils and low lymphocytes, it’s a clear sign that your immune system is out of balance. This pattern often points towards chronic inflammation, a key driver of accelerated aging. Recognising this imbalance is the first crucial step towards getting your long-term health and longevity back on track.
Your Body's Immune Defenders: Responders vs. Strategists
Think of your immune system as a highly sophisticated security team protecting your body. For this team to be effective, it needs different specialists for different jobs. Two of the most important players are the neutrophils and the lymphocytes, each with a very distinct and vital role.
Neutrophils are the energetic ‘first responders’ of your immune system. Like firefighters rushing to a blaze, they’re the first on the scene of an injury or infection. They make up the largest portion of your white blood cells—typically 55-70%—and their job is fast, aggressive, and direct. They swarm the area to contain threats, swallowing up bacteria and damaged cells, which creates inflammation—the body’s way of cordoning off a problem area.
On the other hand, lymphocytes are the calm ‘intelligence agents’ of the operation. Making up about 20-40% of your white blood cells, they work with precision and memory. They don’t just react; they learn. Lymphocytes identify specific invaders, create tailored plans to eliminate them, and remember those threats for years. This long-term surveillance is absolutely critical for fending off future illnesses and maintaining order over your lifetime.
Neutrophils vs Lymphocytes: A Quick Comparison
To really understand how these cells work together, it helps to see their roles side-by-side. Here’s a quick summary of what makes each of them unique.
| Feature | Neutrophils (The First Responders) | Lymphocytes (The Intelligence Agents) |
|---|---|---|
| Primary Role | Immediate, rapid response to infection or injury. | Targeted, specific defence and long-term immunity. |
| Part of Immune System | Innate (non-specific, always ready). | Adaptive (learns and remembers specific threats). |
| Typical Percentage | 55-70% of white blood cells. | 20-40% of white blood cells. |
| Response Speed | Very fast – arrives at the scene within minutes. | Slower to activate but provides a lasting response. |
| Key Function | Engulf and destroy pathogens (like bacteria). | Produce antibodies and coordinate the immune attack. |
| Lifespan | Very short – typically a few hours to a few days. | Long-lived – can last for years, providing "memory". |
This table highlights the crucial difference: neutrophils handle the immediate chaos, while lymphocytes provide the long-term strategy and memory needed for lasting health.
This visual shows the typical distribution of these key white blood cells and their distinct roles in your body's defence system.
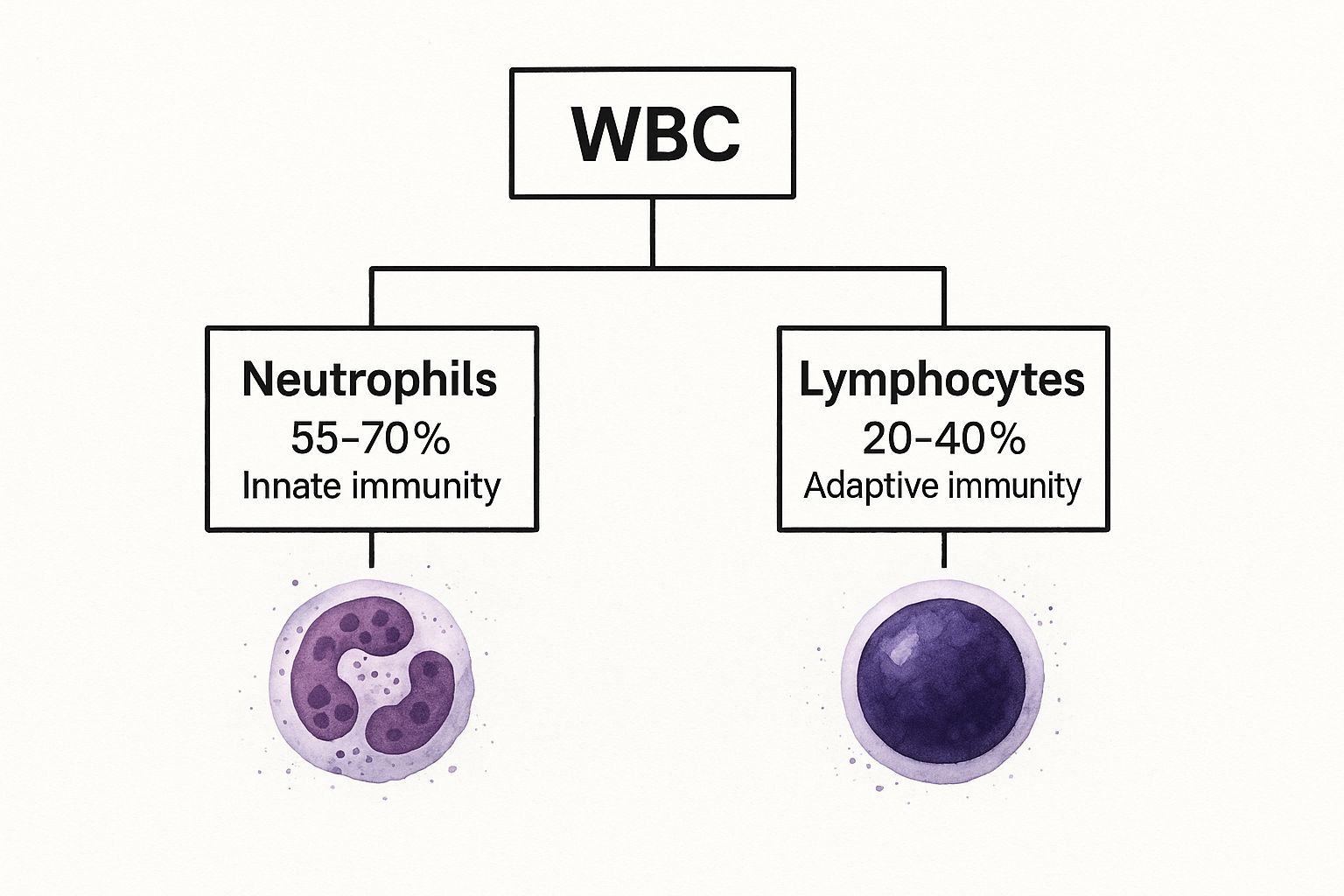
As you can see, neutrophils form the bulk of your immediate defence force, while lymphocytes offer the specialised, adaptive protection that is so vital for your long-term resilience.
When an Emergency Becomes a Habit
In a healthy system, there's a careful balance between these responders and strategists. The problem starts when you have consistently high neutrophils and low lymphocytes. This disrupts the harmony. It tells us that the first responders are constantly being deployed, which is a hallmark of chronic, low-grade inflammation.
This perpetual state of emergency diverts energy and resources away from the strategic, long-term work of the lymphocytes.
This imbalance—too much immediate reaction and not enough strategic oversight—is a critical marker for health. It means the body is perpetually fighting fires, which over time, can wear down its fundamental structures and accelerate the ageing process.
Understanding this dynamic is key. It’s about more than just fighting off the occasional cold; it’s about building a resilient system that supports a long and healthy life. By proactively monitoring your immune health, you can take steps to shift the balance back towards stability.
If you're interested in a deeper analysis, exploring comprehensive testing kits for your immune system can provide invaluable insights into your body's unique needs.
Decoding Your Neutrophil to Lymphocyte Ratio
While looking at individual cell counts gives us some useful clues, the real story about your health emerges when we put them together. The Neutrophil-to-Lymphocyte Ratio (NLR) is a surprisingly powerful calculation that acts like a barometer for your body’s internal stress and inflammation levels. It's more than just a headcount of cells; it's an actionable snapshot of how your immune system is behaving right now.
Imagine your immune system as a seesaw. On one end, you have neutrophils, your fast-acting emergency crew. On the other, you have lymphocytes, your strategic, long-term defence force. In a healthy body, this seesaw stays pretty level, only tilting when it needs to deal with a threat before settling back into balance.
But when you have persistently high neutrophils and low lymphocytes, that seesaw gets stuck. The neutrophil side is way up in the air, and the lymphocyte side is pinned to the ground. This imbalance is a major red flag for your long-term health and longevity.

Calculating Your NLR: A Simple Formula
Working out your NLR is refreshingly simple and uses data from a standard blood test. The formula is just your absolute neutrophil count divided by your absolute lymphocyte count. If you want a deeper dive into all the components, you can learn more by understanding your full blood count results in our comprehensive guide.
NLR = Absolute Neutrophil Count ÷ Absolute Lymphocyte Count
Let's take an example. If your neutrophil count is 6.0 x 10⁹/L and your lymphocyte count is 1.5 x 10⁹/L, your NLR would be 4.0. That one little number tells us an awful lot about the pressure your immune system is under.
What Is a Healthy NLR?
Although the exact numbers can vary a little, a healthy NLR for an adult is generally thought to be between 1.0 and 3.0. This range suggests your immune system is in a state of equilibrium, with a good balance between its emergency responders and its strategic defenders.
An NLR in this sweet spot is a great sign. It indicates your body isn’t fighting significant underlying inflammation. This is exactly where you want to be for longevity, as it lets your body focus its energy on repair and maintenance, not on constantly putting out fires.
Ultimately, a lower NLR reflects a well-regulated, resilient immune system—a cornerstone of healthy ageing.
Why a High NLR Is a Concern for Longevity
When that ratio starts to creep above 3.0, it signals that something is out of kilter. A consistently high NLR is a strong indicator of systemic inflammation, which is a primary driver behind nearly every major age-related chronic disease. This pattern of high neutrophils and low lymphocytes points to two key problems affecting your healthspan:
- Constant Emergency Mode: High neutrophils mean your body is perpetually sending out its first responders. Being in this state of chronic alert drains energy and resources, leading to cellular wear and tear over time.
- Weakened Strategic Defence: Low lymphocyte levels mean your body’s ability to mount a targeted, intelligent defence is weakened. This leaves you more vulnerable to infections and less capable of spotting and eliminating rogue cells before they cause bigger issues.
This chronic imbalance creates an internal environment that can actually speed up the ageing process. It's a clear sign that your body's resources are being diverted to manage immediate, low-grade threats at the expense of long-term health and repair. So, understanding and addressing a high NLR isn't just about fixing a current problem—it's a proactive strategy for investing in a longer, healthier life.
What Causes High Neutrophils and Low Lymphocytes?

Knowing that your immune system is off-kilter is one thing. Understanding why is where you really start to take back control. The pattern of high neutrophils and low lymphocytes isn't just random; it's often a direct response to both short-term triggers and, more importantly for longevity, the chronic lifestyle pressures that keep your body stuck in a state of high alert.
Some of these triggers are brief and your body handles them perfectly. For instance, if you get a bacterial infection or a minor injury, your body will quite rightly flood the area with neutrophils to fight off the invaders and clear away damaged tissue. This is a healthy, appropriate response. Once the threat is gone, your immune system should reset, bringing the balance between neutrophils and lymphocytes back to normal.
The real trouble for our long-term health starts when this imbalance isn't a temporary blip, but becomes the new status quo. This is rarely caused by a single event. Instead, it’s driven by the persistent, low-grade stresses of modern life that slowly wear down our resilience and set the stage for age-related decline.
Chronic Lifestyle Factors Fuelling the Imbalance
The most powerful drivers of a stubbornly high Neutrophil-to-Lymphocyte Ratio (NLR) are often woven into our daily routines. These factors create a smouldering fire of chronic inflammation, which forces your body to constantly pump out emergency responders (neutrophils) while neglecting its more strategic, long-term defenders (lymphocytes).
-
A Diet High in Processed Foods: Think of highly processed foods, refined sugars, and unhealthy fats as constant irritants. They provoke an inflammatory reaction in your gut and across your body, sending a continuous signal to your bone marrow that there's a threat needing a constant supply of neutrophils.
-
Persistent Psychological Stress: When you're constantly stressed, your body is swimming in the hormone cortisol. Cortisol plays a double agent with your immune system: it ramps up the release of neutrophils from your bone marrow while actively suppressing the production and function of your lymphocytes. This directly engineers the "high neutrophil, low lymphocyte" pattern.
-
Poor or Insufficient Sleep: Sleep is prime time for your body's repair crew. Skimping on quality sleep is a major physiological stressor that disrupts immune regulation, drives up inflammatory markers, and stops your lymphocyte population from recovering and doing its vital surveillance work.
-
Excess Body Fat (Adipose Tissue): Fat tissue, especially the visceral fat that cushions your organs, isn't just sitting there. It's metabolically active, churning out inflammatory proteins called cytokines. This creates a non-stop, low-level inflammatory hum that keeps neutrophil production ticking over 24/7.
This constant state of emergency is incredibly draining. It means your immune system is always fighting yesterday's battles, leaving it ill-equipped to handle the challenges of tomorrow.
How Stress Directly Skews Your Immune Ratio
Let's zoom in on stress. Picture your immune system's production centre as a factory with two main assembly lines: one for neutrophils and one for lymphocytes. Under normal conditions, both lines run smoothly. But when the stress hormone cortisol comes flooding in, it's like a frantic factory manager starts barking new orders.
The manager shouts, "Emergency! Shut down the long-term projects and get every worker on the immediate response line, now!" In response, the factory cranks the neutrophil line up to maximum output. At the same time, it shuts down the lymphocyte line, telling those highly specialised workers to stand down.
Over time, this constant emergency footing, driven by cortisol, creates a surplus of reactive neutrophils and a critical shortage of strategic lymphocytes. Your body loses its ability to mount a sophisticated, targeted defence, leaving it vulnerable.
This hormonal command is one of the main reasons a high NLR is so tightly linked to chronic stress. It’s the direct biological fallout of your body being locked in a "fight or flight" mode—a state that's completely unsustainable for long-term health and a fast track to accelerated ageing.
The Long-Term Impact on Your Longevity
When these lifestyle factors become your daily reality, the consequences ripple far beyond a single blood test result. The relentless overproduction of neutrophils and suppression of lymphocytes takes a direct toll on your healthspan—the number of years you live in good health.
Here’s exactly how this imbalance sabotages your efforts to live a long, healthy life:
- Accelerated Cellular Damage: In their mission to destroy threats, neutrophils release powerful enzymes and reactive oxygen species. When this happens constantly due to chronic inflammation, this "friendly fire" starts damaging your own healthy tissues, speeding up cellular ageing.
- Weakened Immune Surveillance: With fewer lymphocytes on patrol, your body gets worse at spotting and eliminating pre-cancerous cells or clearing out stubborn viral infections. Both of these functions are absolutely critical for heading off age-related diseases.
- Resource Depletion: Keeping your body on high alert is metabolically exhausting. It diverts precious energy and nutrients away from essential repair and regeneration processes, which only contributes to a faster decline.
Ultimately, seeing a pattern of high neutrophils and low lymphocytes isn't just about the numbers. It's a clear signal that your lifestyle is actively working against your longevity. Recognising these root causes is the first, most powerful step you can take to rebalance your system for a longer, healthier future.
How a High NLR Impacts Your Long-Term Health
So, we know lifestyle choices can throw your neutrophils and lymphocytes out of balance. But what does that really mean for your health in the long run? Understanding this imbalance—measured by the Neutrophil-to-Lymphocyte Ratio (NLR)—is crucial, because it opens a window into the chronic, low-grade inflammation that quietly speeds up the ageing process.
Think of this persistent inflammation as a slow-burning fire inside your body. Instead of putting out small threats and then switching off, it just keeps smouldering, causing widespread damage over time. This process, which scientists call "inflammageing," is now seen as a root cause of most major age-related diseases. When your immune system is stuck in this high-alert state, it creates the perfect environment for chronic conditions to develop and thrive.
A consistently high NLR shows your body is churning out neutrophils, which release powerful chemicals to fight perceived threats. When this happens around the clock, these chemicals start harming your own healthy tissues, especially the delicate lining of your blood vessels. This sustained, friendly-fire damage is a major reason why an elevated NLR is so tightly linked to cardiovascular problems.
The Cardiovascular Connection
Your heart and blood vessels are particularly vulnerable to the relentless effects of chronic inflammation. A high NLR signals an internal environment that encourages the growth and instability of atherosclerotic plaques—those fatty deposits in your arteries that can lead to heart attacks and strokes. The constant storm of inflammatory signals makes these plaques more fragile and likely to rupture, which can trigger a dangerous blood clot.
This isn't just a theory; it's backed by large-scale studies. A major genetic and epidemiological analysis of 396,020 UK Biobank participants found clear links between a person's NLR and their cardiovascular risk. The research confirmed that a high NLR is a clinically important marker for inflammation-driven heart disease in the UK population.
You can think of a high NLR as an early warning system for your heart. It flags underlying inflammatory stress long before your cholesterol levels might ring any alarm bells, giving you a powerful, proactive tool for prevention.
Beyond the Heart: Metabolic Health and Cellular Damage
The ripple effects of high neutrophils and low lymphocytes don't stop at your circulatory system. This inflammatory state also messes with how your body manages energy and communicates on a cellular level, paving the way for metabolic problems and faster ageing.
This imbalance is closely tied to several other long-term health risks:
- Metabolic Disorders: Chronic inflammation is a well-known driver of insulin resistance, where your cells start ignoring the signals from insulin. This is a direct stepping stone to type 2 diabetes and metabolic syndrome.
- Cellular Ageing: With fewer lymphocytes on patrol, your body’s “immune surveillance” team is understaffed. It becomes less effective at clearing out old, dysfunctional (senescent) cells, which in turn pump out even more inflammatory signals, creating a vicious cycle of ageing.
- Impaired Repair: Your body has a limited budget of resources. When it’s constantly funnelling energy into fuelling an overactive inflammatory response, there’s less left over for the vital repair and regeneration work that keeps you healthy and resilient.
Another really useful marker to track alongside your NLR is High-Sensitivity C-reactive Protein (hs-CRP). The liver produces this protein when inflammation is present, so testing for it gives you another layer of insight. You can learn more about the hs-CRP test and see how it complements your NLR results.
When thinking about all the ways a high NLR can affect your wellbeing, it’s impossible to ignore the profound health benefits of quality sleep. Poor sleep is a massive driver of inflammation and can directly push your NLR higher.
Ultimately, your NLR is a crucial piece of the longevity puzzle. It shows you how your daily choices directly influence the invisible processes that determine how well you age. By treating this simple blood test as a proactive health tool, you can shift from just reacting to problems to actively building a foundation for a longer, healthier life.
Using Your NLR to Understand Cancer Outcomes
While a high Neutrophil-to-Lymphocyte Ratio (NLR) is a strong sign of chronic inflammation in general, it takes on a whole new level of importance in oncology. If you're navigating a cancer diagnosis, this simple biomarker offers a window into how the disease might progress. The pattern of having neutrophils high and lymphocytes low is now widely seen as a valuable tool for understanding the body's internal battle.
A consistently high NLR often suggests a more aggressive disease. Think of it like this: the high neutrophil count shows that your body is in a state of intense, widespread inflammation. This isn't just a side effect—this inflammation can actually create an environment that helps tumours grow, multiply, and spread.
At the same time, the low lymphocyte count signals a serious weakness in your defences. Lymphocytes, particularly your T-cells, are the special forces of your immune system, trained to hunt and destroy cancer cells. When their numbers are low, it means your immune response is compromised and less able to fight back effectively.
The Two-Fold Challenge in Oncology
This imbalance creates a double-edged sword. On one side, you have the body's inflammatory response unintentionally fanning the flames and helping the cancer thrive. On the other, your primary cancer-fighting team—the lymphocytes—is understaffed and struggling to keep up.
This is precisely why a high NLR is so often linked to poorer outcomes across many types of cancer. It tells us that the body's defences aren't just failing to contain the disease, but might be actively working against you. This simple biomarker gives clinicians a much clearer picture of the biological landscape they're up against.
In an oncology setting, a high NLR suggests the odds are stacked against you. The body's inflammatory response is helping the tumour, while its specialised anti-cancer defences are running low. This creates a huge challenge for both the patient's immune system and their treatment plan.
Understanding this helps explain why keeping an eye on your NLR throughout your treatment journey can be so important.
Your NLR as a Prognostic Marker
The predictive power of the NLR in cancer care is backed by a mountain of clinical research. Tracking this ratio gives a real-time view of your immune status and inflammation levels, which can be incredibly useful for making treatment decisions. For instance, a rising NLR might suggest a treatment isn't working as well as hoped, while a falling NLR can be a great sign of a positive response.
A landmark 2012 study from Scotland, which looked at data from 27,031 patients with various cancers, drove this point home. The results were clear: an NLR above a 4:1 ratio was directly linked to significantly worse cancer-specific survival. Of the 7,366 deaths recorded in the study, a staggering 84% were due to cancer, confirming that this simple ratio is a powerful predictor. You can read the full 2012 study on cancer prognosis for a deeper dive.
This evidence shows how a routine blood test can provide critical, life-saving information. By understanding what it means to have neutrophils high and lymphocytes low, you and your medical team are better prepared to tackle the complexities of cancer treatment, turning a simple number into a strategic advantage in the fight for your health.
Actionable Steps to Rebalance Your Immune System for Longevity

Realising that a high Neutrophil-to-Lymphocyte Ratio (NLR) is a red flag for chronic inflammation is the first step.
The next, and far more empowering, step is to do something about it. The good news is that the main drivers behind this imbalance—especially the high neutrophil, low lymphocyte pattern—are often rooted in your lifestyle. This puts you firmly in the driver's seat.Think of this as your practical guide to taking back control. By focusing on proven strategies across diet, stress resilience, and movement, you can actively dial down inflammation and nudge your immune system back into a healthier equilibrium. It’s a profound investment in your future wellbeing.
Embrace Anti-Inflammatory Eating
Your diet is one of the most powerful tools you have for managing inflammation. What you eat can either fan the flames of inflammation or help to extinguish them. The goal is to consistently choose foods that soothe your immune system, not provoke it.
An anti-inflammatory eating plan isn't about harsh restrictions; it's about adding an abundance of whole, nutrient-packed foods that give your body exactly what it needs to thrive.
Foods to Prioritise:
- Omega-3 Rich Foods: Fatty fish like salmon, mackerel, and sardines are loaded with omega-3s, which are powerful anti-inflammatory agents. Try to get at least two servings in per week.
- Colourful Fruits and Vegetables: Think berries, leafy greens, broccoli, and peppers. They’re full of antioxidants and polyphenols that fight off oxidative stress, a major contributor to inflammation.
- Healthy Fats: Avocados, olive oil, nuts, and seeds provide the healthy monounsaturated fats that support your cells and help lower inflammatory markers.
- Fibre-Rich Foods: Legumes, whole grains, and vegetables are crucial for feeding the good bacteria in your gut. A healthy gut is absolutely essential for a well-regulated immune system.
For anyone looking to make personalised dietary changes, exploring resources that offer tailored guidance can be a game-changer. Some people find success with tools like AI-powered meal planning to help build sustainable, healthy habits.
Foods to Minimise:
- Refined Sugars and Grains: Sweets, sugary drinks, and white bread cause sharp spikes in blood sugar, which can trigger an inflammatory response.
- Processed and Fried Foods: These often contain unhealthy trans fats and other compounds (known as AGEs) that are highly inflammatory.
Build Your Stress Resilience
Chronic stress is a key villain behind a high NLR. When your body is constantly swimming in the stress hormone cortisol, it directly encourages that unhealthy "high neutrophils, low lymphocytes" pattern. Building resilience isn't about avoiding stress altogether—that's impossible. It's about getting better at handling it.
"Managing stress is not just about mental wellbeing; it's a physiological necessity. A calm nervous system supports a balanced immune system, which is a cornerstone of longevity."
Simple, consistent practices can make a huge difference in lowering your baseline stress and, in turn, your inflammation.
Strategies for Stress Resilience:
- Mindfulness and Meditation: Even 5-10 minutes of daily mindfulness can help regulate your stress response, lowering cortisol and calming your nervous system.
- Prioritise Quality Sleep: Aim for 7-9 hours of good-quality sleep a night. This is when your body does its critical immune-regulation and repair work, helping to restore lymphocyte levels.
- Establish a Consistent Routine: A predictable daily schedule for sleeping, eating, and working reduces feelings of chaos and gives your body a sense of stability, lowering chronic stress.
Move with Purpose and Strategy
When it comes to inflammation, physical activity is a bit of a double-edged sword. The right amount and type can be powerfully anti-inflammatory, but too much high-intensity exercise without enough rest can actually make things worse. The key is to be balanced and strategic.
A well-rounded routine will support your immune health without tipping your body into a state of chronic stress.
Your Weekly Movement Plan:
- Moderate Cardiovascular Exercise: Aim for 150 minutes a week of things like brisk walking, cycling, or swimming. This gets your circulation going and helps reduce systemic inflammation.
- Strength Training: Squeeze in 2-3 sessions a week. Building muscle improves your metabolic health, which has a natural anti-inflammatory effect.
- Active Recovery: Don't skip the gentle stuff like yoga or stretching. These activities help lower cortisol and promote recovery, which is just as important as the workout itself.
By focusing on these three pillars—eating well, managing stress, and moving smart—you create an internal environment that fosters balance, not chaos. Taking these actionable steps empowers you to lower your NLR, reduce chronic inflammation, and actively build the foundation for a long and vibrant life.
At Lola, we believe that understanding your body's unique data is the first step toward optimising your health for the long run.
Our at-home blood tests provide the clarity you need to track your progress and make informed decisions. Start your journey to better health today at https://lolahealth.com.

