Imagine your body has an internal alarm system. That’s cortisol. It’s brilliant for giving you that jolt of energy and focus when you need to handle a genuine threat—the classic "fight-or-flight" response. But what happens when that alarm gets stuck in the 'on' position? This is the essence of high cortisol.
It’s a state of constant, low-grade emergency that, over time, can seriously undermine your health and chip away at your longevity.
What is High Cortisol? Your Body's Constant Alarm Bell
Think of it like a car alarm that just won’t quit. For a few moments, it serves its purpose, alerting you to a potential problem. But if it blares for hours on end, it becomes a massive nuisance. The constant noise is jarring, the battery drains, and eventually, the car's electronics start to fail. This is a powerful analogy for what chronically high cortisol does to your body.
When cortisol levels are constantly elevated—a condition known as hypercortisolemia—it’s like that incessant alarm. It’s a signal that your body believes it's under siege, whether the threat is real or just perceived. This perpetual state of alert wears down your internal systems, accelerates cellular ageing, and throws off the delicate hormonal balance you need for a long and healthy life.
The Natural Rhythm of Cortisol
Healthy cortisol levels aren't static; they have a natural daily flow called a diurnal rhythm. This internal clock is absolutely fundamental to managing your energy, recovery, and long-term vitality.
Here’s how it’s supposed to work:
- Morning Peak: Cortisol is at its highest around 30-60 minutes after you wake up. This is your body's built-in espresso shot, making you feel alert and ready to take on the day.
- Gradual Decline: As the day progresses, your cortisol levels should steadily fall. This gradual tapering off helps your body shift from a state of doing to one of unwinding.
- Nighttime Low: By the time you go to bed, cortisol should hit its lowest point. This dip is crucial. It’s the green light for your body to sink into deep, restorative sleep and kickstart its cellular repair and recovery processes—the foundation of longevity.
This elegant rise and fall is a cornerstone of good health. The problem starts when the alarm never gets a chance to switch off, breaking this rhythm and robbing your body of its chance to truly rest and repair.
When Cortisol Levels Become a Problem
A healthy resting cortisol level usually sits somewhere between 100-200 nmol/L. When your levels are consistently higher than this, it’s a red flag for chronic stress and a genuine risk to your long-term healthspan.
Just how serious is it? A 2021 study of UK patients offered a sobering look. It revealed that individuals with cortisol levels over 744 nmol/L had significantly worse health outcomes and shorter survival times. You can read more about these findings on the Imperial College London’s news site. This really underscores that high cortisol isn't just a sign of stress; it's a critical marker of physiological strain that can shorten your life.
Ultimately, getting a handle on this hormone is about more than just feeling less stressed. It’s about safeguarding your future. Rebalancing your cortisol is one of the most fundamental actions you can take to enhance your vitality and extend your healthspan.
What’s Really Driving Your High Cortisol?
It’s easy to just blame "stress" for high cortisol, but that word alone doesn't really get to the heart of the matter. To truly understand what’s going on, we need to look at the specific triggers that are keeping your body’s alarm system permanently switched on. Think of them as constant inputs feeding your stress response, each one nudging your hormones further out of balance and potentially chipping away at your long-term health.

By breaking down these drivers into clear categories, you can start connecting the dots between your daily life and your hormonal health. This is the first practical step towards reclaiming balance and building a solid foundation for a longer, healthier life.
The Pressure Cooker of Modern Life
The most obvious culprit, of course, is chronic psychological stress. This isn't about the short-term challenges that come and go; it's the relentless, day-in, day-out pressure that so many professionals and high-achievers know all too well.
A demanding career, with its endless deadlines and a constant barrage of notifications, creates a state of perpetual high alert. Your body doesn’t know the difference between a predator and an overflowing inbox—the adrenal glands just get the signal to pump out cortisol. Over time, this sustained output completely disrupts your natural hormonal rhythm, undermining your body’s ability to repair itself, a crucial process for longevity.
"Your body is designed to handle acute stress and then return to baseline. Chronic stress, however, removes that recovery period, forcing your systems to operate in an emergency state indefinitely. This is where the real damage to long-term health begins."
Personal pressures from financial worries, relationship troubles, or caregiving duties just add more fuel to the fire. When these stressors become a constant backdrop to your life, your body stays on high alert, and cortisol levels never get the chance to return to a healthy baseline.
Physiological Triggers Hiding in Plain Sight
It's not all in your head. Several physical factors can push cortisol levels up, and they are often the ones we overlook in our quest for longevity.
-
Poor Sleep: A bad night's sleep isn't just frustrating; it's a major physiological stressor. When you don't get enough deep, restorative sleep, your body registers it as a threat and ramps up cortisol production the next day. This easily becomes a vicious cycle: high cortisol wrecks your sleep, and poor sleep raises your cortisol, accelerating the ageing process.
-
Overtraining: We all know exercise is good for us, but for driven athletes and fitness enthusiasts, it's easy to push too hard without enough rest. Overtraining, or more accurately, chronic under-recovery, sends a powerful stress signal through the body. The result is persistently high cortisol, muscle breakdown, and a deep sense of fatigue that detracts from your healthspan.
-
Dietary Choices: What’s on your plate directly impacts your hormones. A diet heavy in processed foods, refined sugars, and inflammatory fats sends your blood sugar on a rollercoaster. This metabolic instability is a physical stress that forces your adrenal glands to release cortisol to try and manage the chaos, contributing to age-related diseases.
-
Chronic Inflammation: When your body is fighting a low-grade, persistent battle against things like a poor diet, gut imbalances, or hidden infections, your immune system is always on. A key job of cortisol is to manage inflammation, so when the inflammation becomes chronic, cortisol production goes into overdrive.
Figuring out these hidden drivers is a game-changer. Once you know whether your high cortisol is linked to your sleep, your training, or your diet, you have a clear, actionable starting point. You can learn more about how to check for these imbalances in our guide on at-home hormone level testing.
Medical Conditions and Medications
Finally, it’s crucial to recognise that sometimes high cortisol stems from an underlying medical issue that requires a professional diagnosis.
One such condition is Cushing's syndrome, a disorder caused by prolonged exposure to high cortisol, often due to a tumour on the pituitary or adrenal glands that triggers excessive hormone production.
Certain medications can also be the culprit. In particular, long-term use of corticosteroids like prednisone, prescribed for inflammatory conditions, can artificially elevate your cortisol. It’s absolutely vital to have an open conversation with your doctor about every medication you're taking and how it might be affecting your hormonal health. Pinpointing the true driver is the only way to create a plan that actually works.
The Telltale Signs of Chronically High Cortisol
When your body's stress alarm is stuck in the 'on' position, it doesn't just buzz quietly in the background. Chronically high cortisol sends out a whole cascade of signals, affecting nearly every system you rely on to feel sharp, energised, and healthy. These symptoms aren't just minor annoyances; think of them as critical warning lights on your dashboard, signalling that your body is under an unsustainable amount of strain that can shorten your healthspan.
Learning to spot these patterns is the first real step toward getting back in the driver's seat. You'll start to see how seemingly random issues—like that stubborn belly fat and your inability to focus—might actually be connected to a single hormonal root cause. It's about seeing the bigger picture of what high cortisol is doing to your body and your long-term health.
Metabolic and Physical Signs
Often, the most obvious signs of high cortisol show up on the outside, driven by some pretty profound changes to your metabolism. These physical symptoms are the direct result of cortisol messing with how your body stores energy and repairs itself, basically fast-tracking the ageing process from the inside out.
One of the classic complaints is stubborn weight gain, especially around the abdomen. High cortisol encourages the storage of visceral fat—that’s the dangerous stuff that wraps around your internal organs—and it’s notoriously tough to shift with just diet and exercise. You might also notice a puffiness in your face (sometimes called "moon face") and extra fat deposits between your shoulder blades.
But it goes deeper than just weight. High cortisol can weaken your body’s very structure. You may experience:
- Muscle Weakness and Loss: Cortisol is a catabolic hormone, which is just a technical way of saying it breaks tissue down. Over time, this leads to muscle wasting (sarcopenia), a key marker of accelerated ageing.
- High Blood Pressure: By making your body more sensitive to other hormones that tighten blood vessels, cortisol can push your blood pressure up, putting you at greater risk for heart disease.
- Thinning Skin: You might find that your skin becomes more delicate, bruising at the slightest knock or taking forever to heal from a small cut.
Cognitive and Mood Signs
Your brain is incredibly sensitive to cortisol. A quick burst can sharpen your focus for a short sprint, but a constant flood does the exact opposite. It degrades your cognitive function and throws your mood off balance, making it incredibly difficult to perform at your best, whether at work or at home.
Many high-achievers I've worked with describe it as a persistent "brain fog." It’s that feeling of mental sludge that makes it hard to concentrate, pull up memories, or think with any real clarity. This isn't a personal failing; it's a physiological response. Your brain is simply overwhelmed by stress hormones.
High cortisol essentially locks your nervous system into a "fight-or-flight" state. This makes it almost impossible to get into the calm, focused headspace you need for deep work, creativity, and keeping your emotions in check. It's a state of chronic alert that poses a direct threat to your long-term cognitive health.
Other key signs to watch for include:
- Anxiety and Irritability: Feeling constantly on edge, snappy, or prone to anxiety is a common side effect of your brain being bathed in stress signals.
- Low Mood or Depression: The relentless pressure of high cortisol can drain your brain of feel-good neurotransmitters like serotonin, contributing to feelings of apathy or even depression.
To give you a clearer overview, here's how these symptoms can manifest across different parts of your body.
Symptoms of High Cortisol Across Body Systems
| System Affected | Common Symptoms |
|---|---|
| Metabolic | Abdominal weight gain, increased appetite for sugar/fat, high blood sugar, insulin resistance. |
| Cardiovascular | High blood pressure, increased heart rate, palpitations. |
| Musculoskeletal | Muscle weakness (especially in limbs), loss of muscle mass, bone density loss (osteoporosis risk). |
| Integumentary (Skin) | Thin, fragile skin, easy bruising, slow wound healing, acne, stretch marks (striae). |
| Cognitive | Brain fog, poor concentration, memory problems, difficulty with executive function. |
| Psychological | Anxiety, irritability, mood swings, depression, feeling overwhelmed. |
| Immune | Frequent colds and infections, suppressed immune response. |
| Sleep | Difficulty falling asleep, waking up in the middle of the night (often 3-4 a.m.), feeling unrefrefreshed. |
Seeing these symptoms laid out like this really highlights how one hormonal imbalance can have such a wide-reaching impact on your overall well-being.
Immune and Sleep Signs
Finally, two of the absolute cornerstones of your health—sleep and immunity—are profoundly disrupted by high cortisol. This double-whammy sabotages your body's ability to recover each night and defend itself against illness, which really speeds up the wear and tear on your system.
A classic sign is a completely messed-up sleep pattern. You might struggle to fall asleep because your mind is racing, or you experience that infamous 3 a.m. wake-up, feeling wide awake for no reason. This happens because your natural cortisol rhythm has flipped; it's peaking when it should be at its lowest point, robbing you of the deep, restorative sleep you desperately need.
That lack of recovery has a direct knock-on effect on your immune system. You'll notice it when:
- You get sick all the time: You seem to catch every cold, flu, or bug that goes around the office.
- Wounds heal slowly: A paper cut or a scrape takes much longer to repair than it used to.
These signs are your body’s way of screaming for help, telling you that its core systems are overloaded. Recognising them for what they are is the crucial first step toward tackling the root cause and getting yourself back on a path to a longer, healthier life.
How to Get a Clear Picture of Your Cortisol Levels
If you’ve been feeling off and suspect high cortisol is to blame, you’re on the right track. But suspicion isn't enough when it comes to your long-term health. To truly understand your body's stress response and protect your longevity, you need solid data, not guesswork.
Figuring out how to test for it can seem a bit complicated at first, but it really boils down to a few key methods. Each test gives you a different piece of the puzzle, and knowing the pros and cons of each will help you make informed decisions about your health.
Why a Single Test Might Not Tell the Whole Story
The go-to starting point is often a morning blood test. It’s useful, but it only gives you a single snapshot in time. Think of it like glancing at the weather at 8 a.m. and assuming it will stay sunny and calm all day—you're missing the bigger picture.
Your cortisol is supposed to follow a natural 24-hour cycle, known as its diurnal rhythm. It should be high in the morning to wake you up and then gradually fall throughout the day, hitting its lowest point around midnight to allow for deep, restorative sleep.
For anyone serious about longevity and peak performance, understanding this rhythm is everything. A single high reading in the morning might be perfectly normal. But high levels late at night? That's a massive red flag that your body isn't getting the downtime it desperately needs to repair and recover. This is exactly why one-off tests can miss the subtle imbalances that quietly chip away at your health over the years.
This decision tree can help you start connecting the dots between how you're feeling and what might be going on inside.
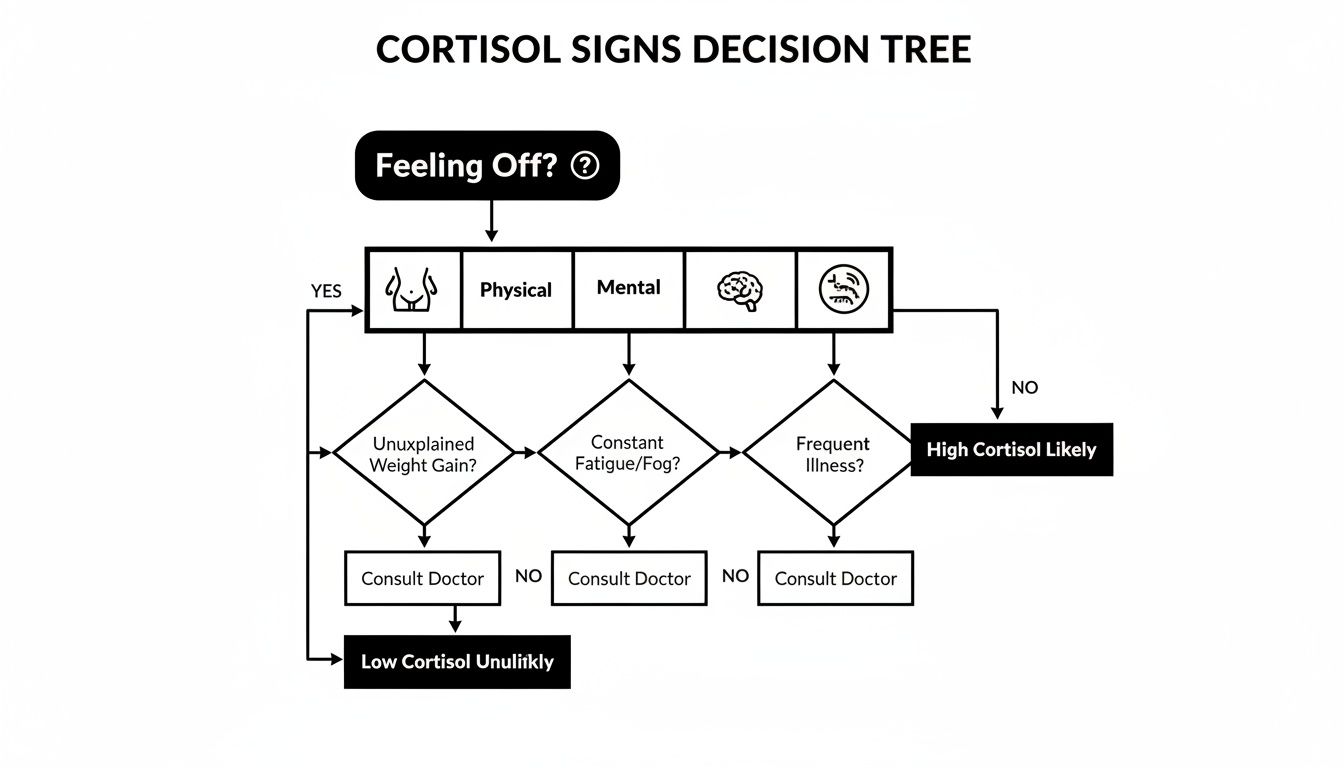
What this shows is that a whole range of symptoms—from stubborn belly fat to persistent brain fog—can all point back to the same hormonal root cause.
Comparing Your Testing Options
To get the full story, healthcare professionals rely on a few different methods. Each has its own strengths for figuring out what’s really driving your cortisol levels.
-
Blood Tests: As I mentioned, this is the standard. It’s great for capturing that morning cortisol peak and is a common first step for screening. It tells you exactly how much cortisol is in your bloodstream at that specific moment.
-
Saliva Tests: This is where things get interesting. Saliva testing is fantastic for mapping out your entire diurnal rhythm. You can easily collect samples at different times—say, morning, noon, evening, and bedtime—to see if your cortisol is following its natural curve. For athletes and busy professionals looking to fine-tune their energy and recovery, this detailed data is gold.
-
24-Hour Urine Tests: This test gives you the big-picture view. By measuring the total cortisol your body gets rid of over a full day, it smooths out the daily peaks and troughs. It's especially useful for diagnosing conditions like Cushing's syndrome, where the body's total cortisol production is consistently through the roof.
By combining different testing methods, you and your doctor can build a detailed, multi-dimensional view of your hormonal health. It’s about moving beyond a single data point to understand the dynamic patterns that truly influence your long-term vitality.
Understanding What Your Results Mean
Getting a lab report back can feel a bit like trying to read a foreign language. Those "normal" ranges are just a guide, and context is everything. What’s considered normal can change based on the lab, the time of day the sample was taken, and your own individual physiology.
Here in the UK, for instance, clinical guidelines are quite specific. Diagnosing adrenal issues often hinges on strict cortisol thresholds set out in NHS protocols. For example, a morning (8-10 a.m.) cortisol level above 300 nmol/L might be used to rule out certain conditions, while a level over 450 nmol/L after a specific stimulation test could be needed to confirm others. These benchmarks are vital for spotting significant problems.
The ultimate goal isn't just to get a number, but to get an actionable insight into your longevity strategy. Whether your results are perfectly in range or flagged as high, they give you a starting point for a targeted plan. You can learn more about how to proactively track your levels by exploring a detailed at-home cortisol test. This puts you in the driver’s seat, allowing you to monitor your progress and see if the changes you’re making are actually working.
Actionable Strategies to Lower Cortisol for a Longer Life
Knowing what drives high cortisol is the first step, but real change happens when you turn that knowledge into action. Managing this powerful hormone isn't about trying to eliminate stress—that's an impossible ask. Instead, it’s about building resilience and creating a lifestyle that gives your nervous system the all-clear signal. By adopting a few targeted, evidence-based strategies, you can start to recalibrate your body's stress response, bring down chronically high cortisol, and build a solid foundation for a longer, healthier life.

This isn’t about a massive, overnight overhaul. Think of this as a collection of practical tools you can weave into your daily routine to gently guide your hormonal rhythm back into a healthy balance.
Master Mind-Body Techniques
Your mind has a direct hotline to your adrenal glands. When you’re feeling mentally frazzled, your body responds by physically pumping out cortisol. The goal of mind-body practices is to interrupt that frantic conversation and tell your body it's safe to stand down.
Practices like mindfulness meditation have been proven to lower cortisol by encouraging a state of relaxed awareness. You don't need to be a guru; even just 10-15 minutes of focused breathing each day can make a world of difference. Try simple box breathing: inhale for four seconds, hold for four, exhale for four, and hold for another four. It’s surprisingly effective.
Another powerful tool is simply spending time in nature, sometimes called 'forest bathing'. Getting out into natural environments has been scientifically linked to lower cortisol, reduced blood pressure, and an overall calmer mindset.
Of course, a big part of lowering cortisol is tackling its primary triggers head-on. This practical guide on how to deal with chronic stress is packed with valuable techniques. These practices aren't just a quick fix; they actively retrain your stress response for better long-term resilience.
Fuel Your Body with Nutrition for Resilience
What you put on your plate directly influences your hormonal landscape. A diet loaded with processed foods and refined sugars sends your blood sugar on a rollercoaster—a physiological stressor that forces your adrenal glands to release cortisol to get things back on track.
The game plan here is to focus on blood sugar stability and anti-inflammatory foods. Build your meals around:
- High-Quality Protein: This is vital for feeling full and preventing those sharp blood sugar swings.
- Healthy Fats: Think avocado, olive oil, and nuts. They help to cool down inflammation in the body.
- Complex Carbohydrates: Fibre-rich foods like vegetables and whole grains give you a slow, steady release of energy.
Foods rich in magnesium (leafy greens, dark chocolate) and vitamin C (citrus fruits, bell peppers) are also great for supporting adrenal health and regulating cortisol. This isn't about a restrictive diet; it's about building a body that's simply less reactive to whatever life throws at it.
Find Your Sweet Spot with Smarter Movement
For ambitious professionals and athletes, it's easy to fall into the "more is always better" trap with exercise. But when your body is already under a heavy stress load, hammering it with gruelling workouts can backfire, sending cortisol levels even higher. The real goal is to find that sweet spot between beneficial movement and overtraining.
High-intensity interval training (HIIT) definitely has its benefits, but it absolutely must be balanced with proper recovery. Pushing yourself too hard without enough rest is a classic recipe for chronically elevated cortisol.
The most effective exercise plan for cortisol management balances intensity with restoration. Think of it as a dialogue with your body—some days you push, and on others, you actively recover. This approach builds strength without burning out your adrenal system.
Make sure to schedule restorative activities into your routine to actively bring cortisol down:
- Yoga and Tai Chi: These practices combine gentle movement with mindful breathing, directly calming the nervous system.
- Walking: A simple daily walk, especially outdoors, is an incredibly effective, low-impact way to reduce stress hormones.
- Stretching and Mobility Work: Releasing physical tension in your muscles can also lower physiological stress.
This balanced approach ensures your workouts are contributing to your longevity, not chipping away at it. For a deeper dive into optimising your routine, have a look at our top tips on hydration, nutrition, exercise, and sleep.
Optimise Your Sleep for Hormonal Reset
Sleep is completely non-negotiable for hormonal health. It’s during deep sleep that your body gets down to its most critical repair work and resets your cortisol rhythm for the day ahead. A bad night's sleep is a massive physiological stressor that all but guarantees an out-of-whack cortisol level the next morning.
Improving your sleep hygiene is one of the highest-impact changes you can make. A simple checklist can get you started:
- Consistent Schedule: Get to bed and wake up around the same time every day—yes, even on weekends. This helps regulate your body's internal clock.
- Create a Dark, Cool Environment: Think cave-like. Blackout curtains and a cool room temperature signal to your body that it's time to power down.
- No Screens Before Bed: The blue light from phones and laptops messes with melatonin production and can throw your cortisol curve off kilter.
- Avoid Late-Night Caffeine and Alcohol: Both can disrupt the deep, restorative sleep cycles your body needs.
All these strategies work together, creating an internal environment where your body can truly thrive. It's a widespread issue, too—UK data from thousands of at-home tests shows an average cortisol level of 370.1 nmol/L, with high levels being linked to the rise of non-communicable diseases. By taking these proactive steps, you can lower your cortisol, boost your resilience, and make a direct investment in a longer, more vibrant life.
Your Questions About High Cortisol, Answered
When you start digging into hormonal health, it’s only natural for questions to pop up. Connecting the dots between how you feel and your body's stress response can feel complex, so let's clear up a few of the most common queries about getting cortisol back in check.
Can High Cortisol Actually Be Reversed?
Yes, absolutely. For the vast majority of people, high cortisol driven by chronic stress isn't a life sentence. Think of it less like a broken part and more like a system that's been running in overdrive for too long. With the right approach, you can absolutely guide your body back to its natural, healthy rhythm.
The whole game is about systematically tackling the root causes. When you start improving your sleep, managing psychological stress with things like meditation or deep breathing, eating whole foods that keep your blood sugar stable, and switching to smarter, more restorative exercise, you’re essentially turning down the volume on your body's alarm system. This gives your adrenal glands a much-needed break, allowing cortisol production to normalise and putting you back on the path to better long-term health.
How Long Does It Take To Lower Cortisol Levels?
That’s the million-dollar question, isn't it? The honest answer is: it depends. There’s no magic timeline. How long it takes to bring cortisol down hangs on a few things—how high your levels are to begin with, how long they’ve been elevated, and how consistently you can stick with new, healthier habits. It’s a process of recalibration, not an overnight fix.
You’ll likely start to feel better within a few weeks of making consistent changes. Maybe you'll notice deeper sleep, a calmer mind, or more even energy throughout the day. But seeing a significant, measurable drop on a lab test? That can take anywhere from a few months to a year. Patience and consistency are your two best friends on this journey.
The goal isn't a frantic, two-week crash course in stress reduction. It's about building sustainable habits that create a new, healthier baseline for your body. This slow-and-steady approach is what builds real resilience.
Focus on small, manageable adjustments you can actually stick with, rather than trying to overhaul your entire life at once. Every positive choice is another step toward restoring your body's balance.
Is High Cortisol From Stress The Same As Cushing's Syndrome?
This is a really important distinction to make. While both conditions involve high cortisol, their origins and severity are worlds apart.
High cortisol from chronic stress is what we call a functional imbalance. Your adrenal system is working correctly, but it’s overproducing the hormone because it’s constantly getting signals of danger from external or internal pressures. It’s a direct physiological reaction to your environment and lifestyle.
Cushing's syndrome, on the other hand, is a specific and much rarer medical condition. It’s usually caused by a tumour—often on the pituitary or adrenal glands—that pumps out massive amounts of cortisol completely on its own, regardless of stress. Its symptoms are typically far more severe and require direct medical intervention, like surgery or medication.
Here’s an analogy: functional high cortisol is like having your house's heating cranked up because the thermostat is set too high. Cushing's syndrome is like the boiler itself being broken and blasting at full power, no matter what the thermostat says. While stress management is good for everyone, if you suspect something more serious is going on, getting a proper diagnosis from a doctor is non-negotiable.
Getting a clear picture of your cortisol levels is a fundamental step toward taking control of your long-term health. At Lola, we make it simple to get the accurate data you need with our professional at-home blood testing services. Stop guessing and start knowing. Learn more and book your test with Lola Health today.
