When you get a blood test for vitamin B12, you'll see your result next to a 'normal range'. In the UK, most NHS labs consider a normal B12 level to be between 180 and 914 nanograms per litre (ng/L).
That’s a pretty wide range, and you'll often see it expressed in different units, too. The equivalent in picomoles per litre is roughly 133 to 675 pmol/L. But what do these numbers really mean for your long-term health, cognitive function, and vitality as you age?
Decoding Your Vitamin B12 Numbers for Longevity
Simply falling within the "normal" range is just the first step. For true longevity and a vibrant healthspan, the goal isn't just to be 'not deficient'—it's to be optimal. A lab result inside the standard window means you're not clinically deficient right now, but it's not a guarantee that your body has what it needs for peak cellular function and long-term resilience.
Think of it like the oil in your car. The 'normal' range on the dipstick means there's enough oil to prevent the engine from seizing. But the 'optimal' level ensures the engine runs smoothly, protecting it from wear and tear for years to come. That's the approach we should take with our B12 levels—aiming for what truly supports our cognitive function and physical energy as we build a foundation for a long, healthy life.
The Key Difference: Normal vs. Optimal
Standard lab ranges are designed to catch clear-cut, clinical deficiencies. The problem for longevity is that many people start feeling the subtle effects of suboptimal B12—like persistent fatigue, declining cognitive sharpness, or nagging brain fog—long before their levels drop into the official 'deficient' zone.
For anyone serious about proactive health and longevity, the focus must shift from simply avoiding disease to actively building resilience. This means maintaining a B12 status that fuels robust cellular repair, sharp cognitive function, and sustained energy—all cornerstones of healthy ageing.
This is a crucial point, especially as we age. While outright deficiency is less common in men, it's a more frequent issue for women of reproductive age, as noted in NHS findings. Real health optimisation means going deeper than the numbers on a page. It's about understanding the longevity blueprint and decoding your vitamins and minerals blood test to ensure your levels are not just acceptable, but genuinely ideal for your long-term wellness.
To make it easier, here's a quick guide to how UK labs generally interpret B12 levels.
A Guide to UK Vitamin B12 Level Interpretation
This table breaks down the different ranges for Vitamin B12 and what they typically indicate.
| Level (ng/L) | Level (pmol/L) | Interpretation |
|---|---|---|
| Below 180 | Below 133 | Deficient: A clear sign of B12 deficiency. Treatment is essential to prevent long-term neurological damage. |
| 180 - 250 | 133 - 185 | Borderline/Grey Area: Symptoms may be present. This is a critical zone for longevity, where proactive steps can prevent future decline. Further testing (like MMA) is often recommended. |
| Above 250 | Above 185 | Normal/Sufficient: Generally considered adequate, though many longevity experts suggest aiming for the upper end of this range for optimal cellular health and cognitive function. |
Remember, this is a general guide. Your individual results and what's "optimal" for you should always be discussed with a healthcare professional who understands your personal health context and longevity goals.
Why Borderline B12 Levels Impact Your Long Term Health

So often, frustrating health symptoms that impact our quality of life begin in the grey area of B12 levels. This is that borderline zone where your result is technically "normal" but might not be anywhere near what your body and brain need to function at their best, day after day, year after year.
Think of it like the oil in a high-performance engine. You wouldn't wait until the warning light flashes to top it up. Running consistently low, even if not empty, causes gradual wear and tear that ultimately affects performance and lifespan. It's the same with B12—a chronic low-level insufficiency can subtly accelerate the ageing process at a cellular level.
The Problem with 'Just Enough'
A lab report that doesn't flag your B12 as deficient doesn't automatically mean you have enough to thrive. In fact, this low-but-not-deficient status is surprisingly common. Research has shown that between 14% and 16% of UK adults show signs of marginal B12 depletion, with levels sitting between 148 and 221 pmol/L. You can explore the research from the National Institutes of Health for a closer look at the data.
This is precisely why you need to listen to your body. Are you dealing with stubborn brain fog, fatigue that never seems to lift, or odd tingling sensations, even though your blood work came back "fine"? These can be early whispers that your cells aren't getting the B12 they need to support your long-term health.
When it comes to proactive health and longevity, the question isn't just, "What is the normal range for vitamin B12?" It should be, "What is the optimal range for my peak performance and long-term health?" Shifting that perspective is the first step towards a longer, healthier life.
These subtle symptoms are your body’s way of signalling it needs support. Understanding the nuances of blood testing for nutrition is crucial for optimising your levels and safeguarding your health for the future. By catching and correcting these borderline issues early, you're making a powerful investment in your cognitive and physical well-being for the decades ahead.
Recognising the Subtle Symptoms of a B12 Imbalance
Connecting how you feel day-to-day with your lab results is one of the most powerful actions you can take for your long-term health. Because vitamin B12 is so fundamental to your nerve function and energy production, even a small dip can show up in ways you might otherwise brush off as just "getting older."
Learning to spot these early clues means you can intervene before a minor imbalance becomes a major problem, a key strategy for extending your healthspan. While the signs of low B12 often overlap, they tend to fall into a couple of main camps.
Neurological and Physical Signs
These are the symptoms you can literally feel in your body. B12 is crucial for maintaining the protective coating (the myelin sheath) around your nerves. When it's suboptimal, communication in your nervous system can falter, leading to physical sensations.
- Pins and needles: That persistent tingling or numb feeling in your hands or feet, known medically as paraesthesia.
- Deep fatigue: This isn’t just feeling a bit tired. It’s a profound exhaustion that a good night’s sleep doesn't seem to fix, draining your energy for daily tasks.
- Balance issues: You might find yourself feeling unsteady on your feet or getting dizzy for no apparent reason.
- A sore or red tongue: This condition, called glossitis, can sometimes be one of the first physical signs that something is off with your B12 levels.
Psychological and Cognitive Shifts
Your brain is an energy-intensive organ that relies on B12 to manufacture neurotransmitters that manage mood and memory. When your supply isn’t optimal, you might notice things feel a bit 'off' mentally, impacting your cognitive longevity.
An unexplained low mood, feeling irritable, or struggling to recall names and facts can all be early signals of a B12 imbalance. Tuning into these mental shifts is just as vital as watching for physical symptoms when it comes to preserving long-term brain health.
It’s worth noting that while less common, exceptionally high B12 levels can also be a red flag. It’s not a sign of supercharged health; instead, it can sometimes point towards an underlying issue that needs a closer look from your doctor. The goal for longevity is always balance and optimisation—not simply more.
Uncovering the Common Causes of Low Vitamin B12
Spotting the symptoms of low vitamin B12 is one thing, but figuring out why your levels have dropped is the key to a sustainable, long-term solution. Low B12 rarely happens out of the blue; it’s usually a signpost pointing to an issue with your diet or, more often, how your body absorbs this crucial nutrient.
Pinpointing the root cause is the only way to get your levels back to where they need to be for good. Simply taking a supplement might patch things up temporarily, but it won’t solve the underlying problem, which could be quietly affecting your health and longevity in other ways.
Autoimmune and Digestive Conditions
In the UK, the leading cause of a serious vitamin B12 deficiency is an autoimmune condition called pernicious anaemia. This is where your immune system attacks the stomach cells that produce a protein called intrinsic factor. Without intrinsic factor, you simply can't absorb B12 from your food, no matter how much you eat. You can read more about this from the Gloucestershire Hospitals NHS Foundation Trust on B12 deficiency causes.
Other digestive conditions can also disrupt absorption, impacting your long-term nutrient status:
- Atrophic gastritis: This involves the thinning of your stomach lining, which reduces stomach acid and intrinsic factor production—a condition that becomes more common with age.
- Coeliac disease or Crohn's disease: Both conditions create inflammation in the gut that can seriously hamper your ability to absorb B12 and other key nutrients from your diet.
Dietary Choices and Medication Effects
What you eat (or don’t eat) and the medications you take can have a huge impact on your B12 levels over your lifetime. People on long-term vegetarian or vegan diets are at higher risk because B12 is almost exclusively found in animal-based foods. Over time, without careful and consistent supplementation, levels can slowly dwindle, affecting everything from your energy to your nerve health.
It's not just about what you eat, but also what you take. Many widely used medications can silently interfere with B12 absorption over time, making this a hidden risk factor that can compromise your health as you age.
Some of the most common culprits are medicines for acid reflux, like proton pump inhibitors (PPIs), and metformin, a front-line drug for managing type 2 diabetes. These can either reduce the stomach acid needed to release B12 from food or interfere with the absorption process itself. Understanding your personal risk factors is the first step towards a productive conversation with your doctor about your long-term health strategy.
How to Get a True Picture of Your B12 Status
A standard serum B12 blood test is a great starting point, but it doesn't always tell the whole story of what’s happening inside your cells. To truly understand your B12 status and how it's affecting your long-term health, we need to look a bit deeper than that single number.
Think of it this way: the standard test is like checking the amount of petrol in your car's tank. It tells you if you have fuel available, but it doesn't tell you if the engine is actually using that fuel efficiently. A "functional deficiency" is when your tank looks full, but the engine is still sputtering—and your long-term health is paying the price.
Beyond Standard Tests: Functional Markers
To see how well your body is putting B12 to work, clinicians often look at functional markers. These substances build up in your blood when B12 isn't doing its job properly. The two most important for assessing your longevity risk are:
- Methylmalonic Acid (MMA): This is often called the gold standard for spotting a functional B12 deficiency. When your cells lack enough active B12 to fuel their mitochondria (the cell's powerhouses), MMA levels in your blood start to climb. Elevated MMA is a direct sign of cellular stress.
- Homocysteine: B12 is essential for converting the amino acid homocysteine into a harmless substance. If B12 is in short supply, homocysteine levels can rise. Elevated homocysteine is a well-known risk factor for cardiovascular disease and cognitive decline, making it a critical marker for longevity.
This flowchart maps out some of the common culprits behind low B12, showing how a proper investigation often involves looking at multiple factors.
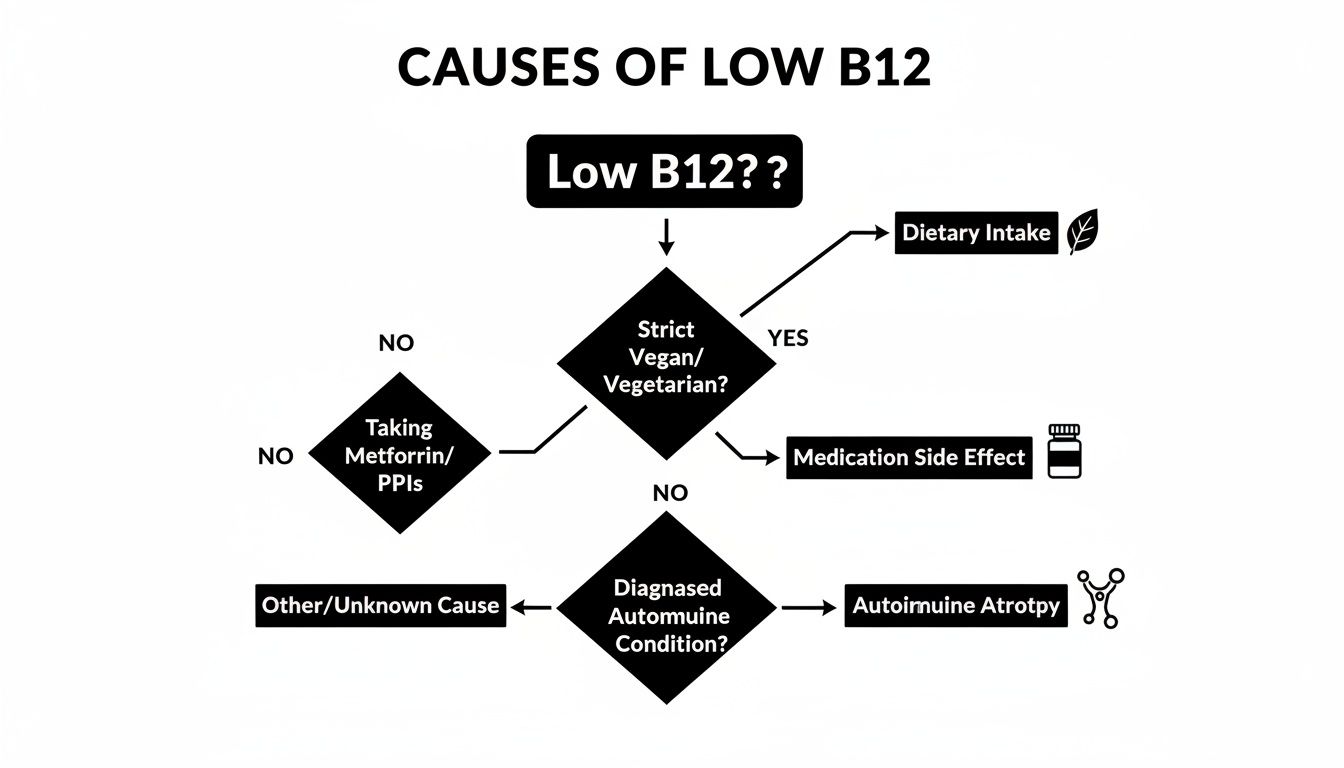
As you can see, issues ranging from diet and medications to underlying autoimmune conditions can all lead to a deficiency, which is why a thorough approach is so important.
Putting It All Together
Looking at these markers together provides a much more accurate and actionable picture. For instance, someone might have a "normal" serum B12 result but show elevated MMA. This combination is a huge red flag, strongly suggesting that their cells are functionally starved of B12, which can silently undermine your health over time. Exploring personalized B12 testing options can help you get this complete view.
The real game-changer for longevity is identifying these functional deficiencies early. Catching a problem at the cellular level allows you to intervene before it leads to the noticeable symptoms we've discussed, safeguarding your energy and cognitive health for the future.
Modern services are making this kind of advanced testing more accessible than ever. With convenient at-home testing, you can gain powerful insights into your cellular health without ever leaving your home. To learn more, check out our guide on ordering a comprehensive blood test for vitamin and mineral deficiency and take control of your proactive health journey.
Your B12 Questions, Answered
Let's dive into some of the most common questions we hear about vitamin B12, so you can feel confident in managing your levels for better health and longevity.
How Often Should I Check My B12 Levels?
If you're healthy and don't have any specific risk factors, getting your B12 checked every two to three years is a sensible approach. But if you're serious about optimising your health for longevity, an annual check is a much better strategy to stay ahead of any decline.
You should definitely consider more frequent testing (e.g., annually) if you:
- Are over 60, as absorption naturally declines with age.
- Follow a vegan or vegetarian diet.
- Live with a digestive issue like Crohn’s or coeliac disease.
- Take certain medications, like metformin for diabetes or PPIs for acid reflux, which can hinder B12 absorption over the long term.
And of course, if you’re already treating a deficiency, your doctor will set up a retesting schedule to track your progress and ensure your levels are restored to an optimal, not just normal, range.
What’s the Difference Between Methylcobalamin and Cyanocobalamin?
Think of it like this: cyanocobalamin is the synthetic, stable form of B12 you’ll often find in fortified cereals and standard supplements. It's effective, but your body must convert it into a form it can actually use, which requires energy and metabolic steps.
Methylcobalamin, on the other hand, is one of the active, 'body-ready' forms of B12. It can get to work right away without needing conversion. For longevity purposes, using an active form can be more efficient, especially for older adults or those with certain genetic variations that make the conversion process less effective. For those exploring different supplement options, you might look into products like Trifolamin B12 lozenges.
Is it safe to take B12 supplements if my levels are normal?
Generally, yes. Vitamin B12 is a water-soluble vitamin, so your body just flushes out what it doesn’t need. While there’s no need for massive doses if your levels are already optimal, taking a maintenance dose to stay in that upper range is generally safe. However, it's always best to chat with your doctor before starting any new supplement, particularly if you have any kidney problems.
Ready to move beyond just 'normal' and discover your optimal vitamin B12 level for a longer, healthier life? With Lola, you can get a comprehensive analysis with a professional at-home blood draw. You'll receive clear, doctor-reviewed results right on our app, starting you on the path to peak wellness. Learn more at https://lolahealth.com.
